EZ-IO Procedure Bone Marrow Aspirate
A development in regenerative medicine is the use of bone marrow derived mesenchymal stem cells for the treatment of degenerative musculoskeletal conditions such as joint osteoarthritis. While the use of autologous stem cells is of immediate interest to all practitioners of regenerative medicine, the complexity and expense of the traditional technique of harvesting bone marrow from the iliac crest and/or adipose fat presents obstacles for practitioners and patients alike. Our purpose here is to propose a novel technique intended to harvest and deliver bone marrow derived mesenchymal stem cells that is at the same time simple, safe, and inexpensive to perform.
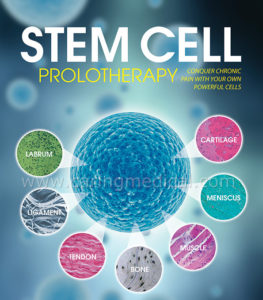
Stem cells, specifically mesenchymal stem cells (MSCs), have been called “patient-specific drug stores for injured tissues” because of their broad range of healing abilities. MSCs are directly responsible for healing damaged tissues after injury. Upon encountering damaged tissue, they release proteins that decrease inflammation, kill invading microbes, and trigger the growth of new connective tissues and blood vessels. In the case of severe damage and cell death, MSCs have the ability to turn into healthy versions of damaged or destroyed cells that they encounter.
When MSCs are taken from whole bone marrow (WBM), and then inject them directly into the problem area, it ‘tricks’ the body into thinking that there has been a new injury without actually causing any tissue insult, creating a second chance at healing. In the case of advanced osteoarthritis where the population of stem cells has been depleted, repopulating the area with stem cells, and thereby restoring the body’s natural ability to begin a therapeutic process.
CONDITIONS THAT ARE BEING INVESTIGATED:
- Osteoarthritis of any joint
- Back Pain (degenerated/dehydrated discs, stenosis, facet arthrosis, SIJ syndrome, sciatica, etc)
- Neck Pain
- Headaches (except true hormonal migraines)
- Sports Injuries (tennis elbow, rotator cuff tear, ACL tear, torn meniscus, chronic ankle sprains, Achilles tendonitis, chronic subluxation/dislocation of shoulder, torn labrum of shoulder or hip, etc)
- Overuse Syndromes (plantar fasciitis, carpal tunnel syndrome, tenosynovitis, TMJ syndrome, etc)
- Avascular Necrosis
- Non-union Fractures
Regenerative therapeutic strategies for joint diseases usually employ either enriched concentrates of bone marrow-derived stem cells, chondrogenic preparations such as platelet-rich plasma (PRP), or irritant solutions such as hyper osmotic dextrose. Here a cost-effective regenerative treatment using direct injection of bone marrow aspirate concentrate (BMAC) into osteoarthritic joints in combination with hyper osmotic dextrose/PRP will be discussed.
Studies of PRP as a treatment for osteoarthritis are becoming more prevalent. Currently numerous publications show PRP to be clinically effective in reducing pain for up to twelve months after injection when a leukocyte poor product is used intra-articularly. Positive outcomes are found more commonly in younger patients with less severe joint osteoarthritic changes.
Bone marrow aspirate concentrate (BMAC) is a rich source of mesenchymal stem cells (MSC), has potential greater than PRP to regenerate cartilage defects via tissue signalling in osteoarthritis, and potentially slow down or improve the disease process. Hyaline cartilage, made up of type II collagen, has no nerve, blood or lymphatic supply. This lack of vascular supply, and other factors such as the inability of resident chondrocytes to migrate to injured areas, limits the healing ability of cartilage as compared to soft tissue and bone. This absence of self-renewal properties has led researchers and clinicians to turn toward the use of autologous MSCs as a potential resource to regenerate damaged tissue in patients who suffer from joint degenerative arthritis.
Prolotherapy is an alternative therapy for treating musculoskeletal pain that involves injecting an irritant substance into damaged connective tissues to promote the growth of new, healthy tissue. Because prolotherapy aims to induce the growth of tissues to repair or replace damaged cartilaginous/tendon structures, it falls into the category of “Regenerative Medicine”. In recent years, many prolotherapists have begun using platelet rich plasma (PRP) in place of irritant solutions to treat conditions such as osteoarthritis (OA) and tendinopathies. Because of its simplicity, safety, and affordability, PRP preparation and delivery is easily introduced into a regenerative medicine practice.
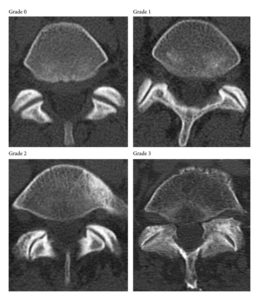
As emerging data supports the percutaneous injection of bone marrow derived mesenchymal stem cells for the regeneration of articular cartilage, Centeno, et al. found that autologous MSCs and percutaneous injection into a knee with symptomatic and radiographic degenerative joint disease resulted in significant cartilage growth, decreased pain, and increased joint mobility(6).
Prolotherapy(7, 8) and PRP(9) have shown promise in the treatment of OA. However, bone marrow aspiration has traditionally been performed in a surgical suite using fluoroscopic guidance with either conscious sedation or general anaesthesia making the procedure more complex than most practitioner offices are equipped for. Iliac crest marrow is then concentrated using commercially available systems, rendering bone marrow aspirate concentrate (BMAC), which is then blended with PRP in order to provide the MSC with growth factors. The complexity of this procedure combined with the expense of the materials makes it cost prohibitive to many patients. Resultantly, some practitioners have sought a method to harvest MSCs for reintroduction that is safe, simple, and inexpensive.

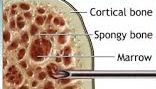
Intraosseous infusion (IO), a technique for vascular access, was first described in 1922 and was widely used for drug administration in pediatric medicine by the 1940s. Its use declined during the 1950s with the advent of single-use intravenous catheters, but re-emerged in the 1980s and today IO is widely used in emergency medicine. A commercially available IO device is the EZ-IO® Intraosseous Infusion System. The EZ-IO is a small, battery-powered, handheld device that drives a beveled, hollow, drill-tipped needle set. It is designed to access the proximal tibia. The EZ-IO provides the non-surgeon easy and rapid access to the intramedullary space and enjoys an excellent safety profile(10).
Some practitioners(1) have injected a blend of autologous bone marrow aspirate concentrate (BMAC) collected from the tibia using the EZ-IO and PRP into shoulder/hip/knee and peripheral joints. Results have been promising and no adverse effects reported beyond injection discomfort and the initial soreness and stiffness normally associated with prolotherapy.
Indications for such procedures have included damaged or degenerated articular surfaces of the shoulder, hip, knee, damaged cruciate ligaments of the knee and peripheral joints. Ultrasound guidance always utilised.
As with any procedure relative and absolute contraindications do apply. In this instance may include, hemorrhagic disorders such as haemophilia and/or use of anticoagulants, skin infections or bone disorders such as osteomyelitis.
Based on results(1), injection of BMAC for osteoarthritis of the knee, hip, shoulder and low back pain appears to be safe and produces consistently satisfactory results.
This series of simple treatment protocols does not claim to provide any hard evidence; it is merely intended as an empirical view of various approaches and procedures being made available in this new and rapidly growing field.
Bone Marrow Aspirate Concentrate for Cartilage Defects of the Knee: From Bench to Bedside Evidence.
Cotter EJ, Wang KC, Yanke AB, Chubinskaya S.
Cartilage. 2018 Apr;9(2)
Bone Marrow Aspirate Concentrate-Enhanced Marrow Stimulation of Chondral Defects.
Madry H, Gao L, Eichler H, Orth P, Cucchiarini M.
Stem Cells Int. 2017;2017
Sampson S, Botto-van Bemden A, Aufiero D.
Phys Sportsmed. 2013 Sep;41(3):7-18.References:
1. Regenerative Injection Therapy with Whole Bone Marrow Aspirate for Degenerative Joint Disease: A Case Series-Ross A. Hauser, MD and Amos Orlofsky, PhD
2. Office-Based Harvest of Mesenchymal Stem Cells by Tibial Intraosseous Cannulation: Journal of Prolotherapy. 2011;3(2):653-657 By Harry Adelson, ND Office-based-harvest-of-mesenchymal-stem-cells-by-tibial-intraosseous-cannulation-part-1
3. Clinical Outcome of Bone Marrow Concentrate in Knee Osteoarthritis Kristin S. Oliver, MD, Matthew Bayes, MD, David Crane, MD, Chakrapani Pathikonda4. Autologous Stem Cell Therapy- A Naturopathic Approach to the Treatment of Chronic Low Back and Discogenic Pain. The Pain Practitioner Dec 2016:26-27. Harry Edelson, ND
5. Autologous Stem Cell Therapy - A Naturopathic Approach For The Treatment Of Chronic Musculoskeletal Pain Conditions—Part ll of ll. The Pain Practitioner Winter 2015:40-43. Harry Edelson, ND
6. Centeno CJ et al. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008; 11:3:343-353.
7. Reeves KD, et al. Randomized prospective double-blind placebo-controlled study of dextrose Prolotherapy for knee osteoarthritis with or without ACL laxity. Alt Ther Hlth Med. 2000;6(2):37-46
8. Reeves KD, et al. Randomized prospective placebo controlled double blind study of dextrose Prolotherapy for osteoarthritic thumbs and finger (DIP, PIP and Trapeziometacarpal) joints: Evidence of Clinical Efficacy. Jnl Alt Compl Med. 2000;6(4):311-320.
9. Kon E, et al. Platelet-rich plasma: intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc. 2010 Apr;18(4):472-479.
10. Ngo AS, et al. Intraosseous vascular access in adults using the EZ-IO in an emergency department. Int J Emerg Med. 2009;2:155-160.