
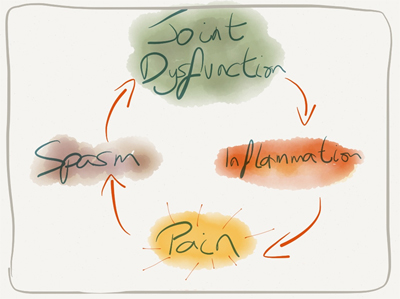
Repetitive superficial low back/cervical spine micro trauma or a significant insult, leading to failure of joint cartilage, causing inflammation accompanied by synovitis, effecting changes in subchondral bone, resulting in the onset of osteoarthritis and associated pain.
So, Superficial injury and fibrillation of articular cartilage as a consequence of ageing, genetic, hormonal or mechanical factors are not necessarily associated with joint pain. However, failure of joint cartilage accompanied by synovitis and abnormalities in subchondral bone and its vasculature generally is, the syndrome being known as osteoarthritis.
Facet Arthropathy
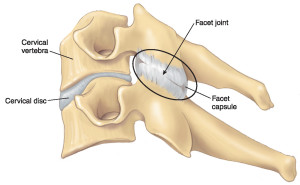
The facet joints are the two joints behind each motion segment. Rotation occurs at these joints in the lumbar spine and flexion in the cervical spine. That is why in the lumbar spine the facet joints are more sagitally oriented to allow for movement in this axis and in the cervical spine they are more coronally oriented to allow for flexion.

The concept of the normal is where the facet joints are kept in a neutral position when a disc has height associated with it. Collapse the disc and the facet joints sublux. Subluxation is a term that simply means non-congruent. In a subluxed position joints are painful and become arthritic.
We suggest that the progression of early cartilage fibrillation to symptomatic OA arises initially as a consequence of the release into synovial fluid of cartilage-derived antigens that activate joint lining macrophages and circulating leukocytes, thereby establishing a synovitis. In healthy cartilage, effective weight-bearing requires a high concentration of intact proteoglycan. Degradation of the cartilage proteoglycan is a key early event in the development of osteoarthritis.

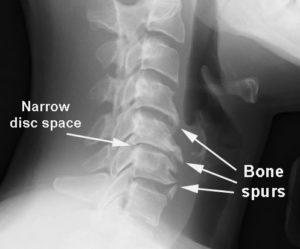
Grade 0 - Indicates normal facets. The gap between the joint is filled with cartilage which is not visible on a CT scan hence appearing as a gap. When the gap is gone you can assume the cartilage is also.
Grade 1 - Mild arthritis, joint space narrowing.
Grade 2 - Moderate, sclerosis.
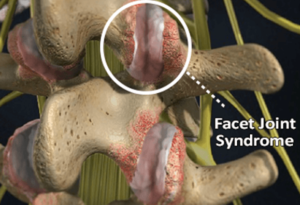
Grade 3 - Severe, osteophytes. Demonstrates a grossly abnormal set of facet joints - defined as abnormal by the ratty appearance to the actual joint, and overgrowth of bone around the joint (osteophytes - the body's attempt to stabilise an abnormal joint by laying down more bone). When the cartilage is gone you have bone rubbing on bone and this is painful. Often the diagnosis of pain secondary to the facet joints is able to be diagnosed with a history. A definitive diagnosis can then made by clinical imaging.
Posterior Facet Syndrome
So, basically Posterior facet syndrome (facet disease) is a degenerative spine condition that occurs when arthritis develops in the facet joints. The facet joints are the pivotal joints that connect the vertebrae and allow them to bend and hinge, giving movement to the spine.
What are symptoms of facet joint problems? Pain, numbness, and muscle weakness associated with facet joint syndrome will affect different parts of your body depending on which of your nerves are being affected.
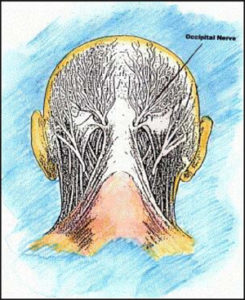
If the nerves affected are in your cervical spine, you may have symptoms in your neck, shoulders, arms and hands. Instability in the cervical spine causes tremendous muscle tension in the paraspinal muscles behind the head which inflames, traps and irritates the greater and lesser occipital nerves. These nerves supply a large portion of the scalp in a balaclava-type distribution and so patients with cervical degenerative joint changes often describe headaches in this typical area. If the headaches seem to be related to mechanical activities where the neck is used, for example poor desk posture, overhead work, lifting above shoulder height etc. then it is likely these nerves are responsible. In this instance the combination of Prolotherapy and Perineurial Injection Therapy may be the treatment of choice.
Prolotherapy and Perineural Injection Therapy
Nerve entrapment and neuritis is seldom considered as a cause of musculoskeletal pain.This can be difficult to diagnose clinically and can be normal on imaging.
If correctly diagnosed this can potentially be successfully treated.
There are certain sites where nerve entrapment is more likely and should be considered when a patient presents with pain in these areas.
Nerves normally glide between muscles and soft tissue with movement. The term paradoxical motion.
With injury the nerves can either get irritated (neuritis) or “stuck” due to surrounding scar tissue. Of course these can occur in combination.
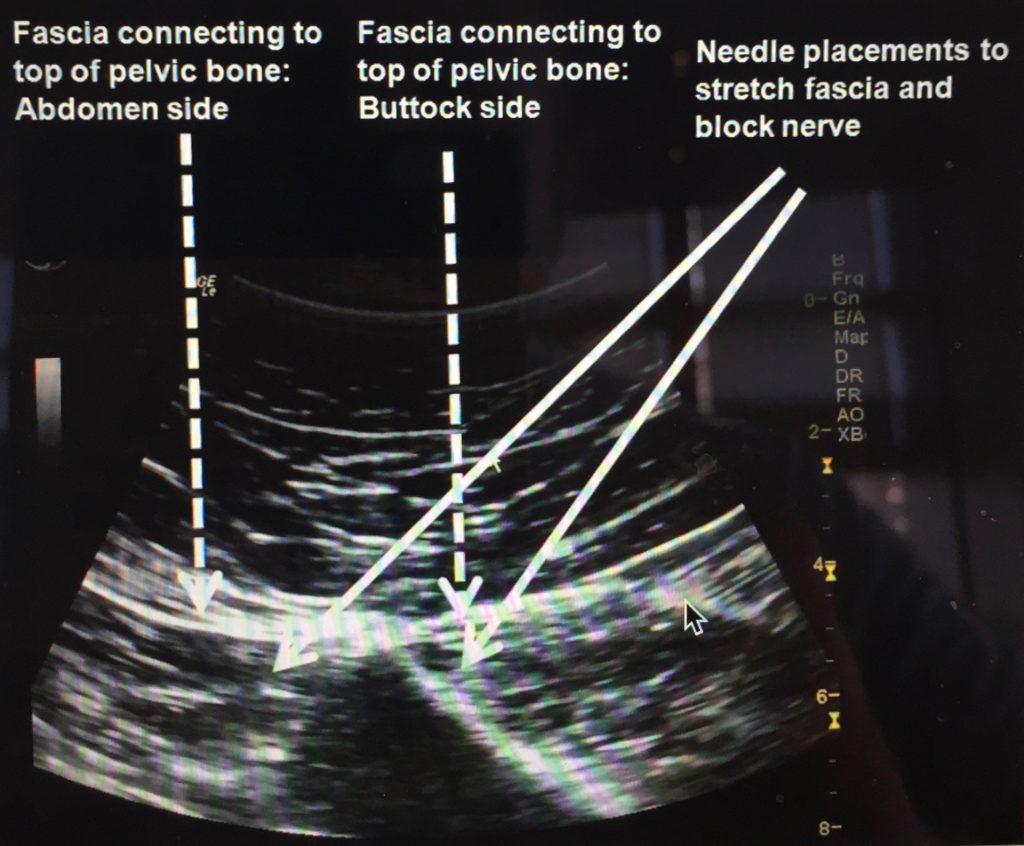
A potential treatment for an entrapped nerve is ultrasound guided neural hydro dissection.
Ultrasound is used to visualise the nerve and a needle is placed next to the nerve (perineurium) and a solution of 5% Dextrose is used to carefully dissect the nerve and mechanically free it from the surrounding tissues.
This is a minimally invasive technique that is surprisingly well tolerated with minimal discomfort (the nerve itself is not touched by the needle).
Nerves that can be potentially entrapped and “freed” include the following:
- Posterior interosseous nerve at the elbow – pain mimicking tennis elbow.
- Lateral cutaneous nerve of the thigh – anterior thigh pain.
- Inferior calcanea nerve and medial calcaneal nerve – mimicking plantar fasciitis.
- Ulnar nerve at the elbow – pain and numbness in 4th and 5th fingers.
- Median nerve – Carpal tunnel syndrome.
- Infrapatellar branch saphenous nerve – medial knee pain and pain mimicking pes anserine bursitis.
- There are nerves can get entrapped such as saphenous nerve, common peroneal nerve.
- Supra scapular / Axillary nerve - shoulder pain.
- Greater/Lesser occipital nerve - neck pain and headaches.
- Sciatic nerve region popliteal fossa - posterior knee pain.
- Sciatic nerve / priformis muscle - sciatica or posterior leg pain.
- Pudendal nerve - pain ischia rectal fossa or pelvic floor.
Briefly again, dextrose injection (15% to 25% concentration) stimulates a brief AA (arachidonic acid) pathway inflammation. AA inflammation is the type of inflammation to which most practitioners are referring when they use that term. After an injury, the body uses primarily AA inflammation to try to repair the damage. With prolotherapy there is no significant damage, because there is no stretching or tearing of fibres, but the body still begins a repair process, which allows the structure to regenerate.
Healing can take months, but some patients get better quickly. This is likely because dextrose D15, D25 also have effects on nerves.
This can be explained by another type of inflammation that has been recognised, and that is called neuropathic inflammation. This type of inflammation is produced by small sensory nerves (The epineurium is the outermost layer of dense irregular connective tissue surrounding a peripheral nerve. It usually surrounds multiple nerve fascicles as well as blood vessels which supply the nerve. Vasa nervorum are small arteries that provide blood supply to peripheral nerves, and these neurons are very needy little things). that are protein producing (“peptidergic”). These nerves normally produce proteins that can be healing or damaging. When produced damaging proteins, if the nerve is irritated that is called “neuropathic inflammation”. Dextrose injection in low concentration (5%) reduces neuropathic inflammation. This does not stimulate AA inflammation; the primary intent is to treat the fascial layers of the perineurium.
There is a protein that sits on the surface of some protein-producing (peptidergic) nerve cells. That protein is called a receptor, because it receives information that causes it to change what the nerve cell does. If the receptor is “mellow” (down-regulated), the nerve cell will be “good” (produce healthy, non-pain producing proteins). If the receptor is “over-active” (up-regulated), then the nerve cell will be “evil/bad” (produce damaging and pain-producing proteins). Thus, this small protein receptor on the surface of the nerve cell is what makes the nerve cell quickly (in seconds) change its character from “good” to "bad.” This receptor is called TRPV-1 (transient receptor potential vanilloid - Type 1). We will call the sensory nerves that are controlled by this receptor “TRPV-1 nerves.” There is a whole “system” of sensory nerves throughout the body, supplying virtually all areas, and is termed the “peptidergic sensory system” because of the ability of these nerves to make proteins (peptides) to affect other structures. The focus will be on these nerves that supply the superficial and deep layers that are now thought to be involved the most in chronic pain. We will call these nerves simply TRPV-1 nerves or “T-nerves.”
When TRPV-1 Nerves Behave Badly – Neuropathic Inflammation
When the TRPV-1 receptor is “over-active” (up-regulated), the TRPV-1 nerve produces proteins that directly cause pain (Substance P, Glutamate are important ones) and proteins that can cause breakdown in all soft tissue structures (CGRP-1 or calcitonin-gene-related peptide). When the TRPV-1 nerves are producing degenerative proteins that damage other structures, it is called Neuropathic (nerve-caused) Inflammation.
Anti-Inflammatory Medications Generally Don’t Work For Neuropathic Inflammation..
Anti-inflammatory medications target the AA-inflammation and often do so by blocking cyclooxygenase. Blocking cyclooxygenase does not affect the N inflammation pathways. Anti-inflammatory medications have some pain-relieving ability other than just by blocking AA inflammation, so they can be useful, although seldom strikingly useful.
How Do Bad Nerves Affect Other Structures
(ie, ligaments, tendons, and cartilage) And Cause Chronic Pain?
Hilton’s Law: States that TRPV1 nerves are ubiquitous and connect to all structures and interconnect with each other. Nerves that cover subcutaneous to deep tissues are joined by nerves from joints, ligaments, and tendons on their way to the spinal cord.
Simply surrounding a nerve around its entire circumference, even without squeezing it, will shut off fast conduction in that nerve, and cause it to behave abnormally. This depiction illustrates how merely touching a nerve on all sides will lead to a swelling reaction. Although the nerve was merely touched, the area can become a point of constriction as the nerve swells on either side of the constriction. Those patients that have heard of Morton’s Neuroma in feet may be interested to know that this is how nerves swell up and become neuromas.
Perineurial Subcutaneous/Deep Injections
It has been clinically observed that injection of 5% dextrose subcutaneously is analgesic to nerve pain, usually completely, and within seconds. This is consistent with a rapid block of that TRPV1 receptor as this occurs without anesthetic included. This typically may need to be repeated but after several treatments leads to progressive benefit, and according to ultrasound follow up shows evidence of stimulating healing of deeper structures.
Injection about a nerve in a deeper region where it has to go around objects or through layers called “fascia” is also utilized, as it is at those points that nerve irritation can occur as well. This dilation by fluid, which had been recently found to be better done with dextrose and lidocaine, is called hydrodissection.
Where Would “Perineurial Deep Injection” (PDI) Be Helpful?
TRPV-1 Nerves are not only irritated when they have to penetrate fascia at the skin level, but also when they have to penetrate layers of fascia in other regions of the body. They may also have to contend with bones and various “tunnels, or passages. Any of these areas can malfunction or be changed in such a way as to “touch” the TRPV -1 nerve.
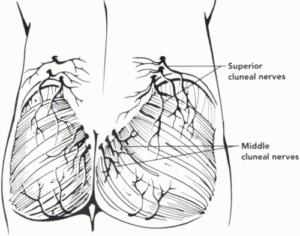
This figure shows a depiction of a nerve for low back pain called the superior cluneal nerve. It passes through a tunnel that is on the top of the pelvic bone but about 25-30mm deep in most people.
This nerve can get trapped or squeezed on either side of the fibro-osseous tunnel.
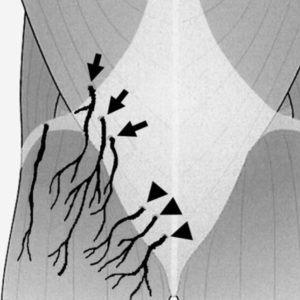
The superior cluneal nerve (arrows) consists of 4-6 nerves; it runs around the paraspinal muscle and penetrates the thoraco-lumbar fascia near the iliac crest before it arrives at the buttock. The middle cluneal nerve is identified by arrowheads
In Summary:
1. The importance of the TRPV-1 receptor as the “faucet” that controls whether a nerve causes pain and why it is so important to “turn down the faucet” (down-regulate) the TRPV-1 receptor.
2. How the ability of nerves to conduct in both directions and their connection with joints and ligaments allows “bad-behaving” nerves to send “breakdown proteins” and “pain proteins” to those structures.
3. Why nerves should not be ignored when treating deeper structures as they are often the underlying cause of damage to those deeper structures.
4. How prolotherapy turns on AA (traditional) inflammation briefly to repair ligament/tendon and turns down N (nerve caused) inflammation to release nerve irritation.
5. How nerves responsible for pain can be treated in several different ways, such as perineurial subcutaneous injection (PSI) or perineurial deep injection (PDI).
Technique of Cellular Prolotherapy..
Prolotherapy is an injection technique whereby certain solutions are injected to cause an inflammatory healing response in part by causing local cellular injury to an area. Dextrose prolotherapy (15% soft tissue, 25% IA) basically works by osmotic action, it’s a hyper-concentrated solution that draws the water out of the cells it comes into contact with causing them to lyse triggering a pro-inflammatory response. Using dextrose solution (15% or 25%) and PRP (platelet rich plasma) together, the platelets will be “lysed” (imploded), larger amounts of growth factors in the platelets will be released into solution. There are clinical situations where this would be an advantage and other times when it would be a disadvantage, but you still end up with a solution that’s likely a net positive to the patient.

Prolotherapy works by causing a temporary, low grade inflammation at the injection site, activating fibroblasts to the area, which, in turn, synthesize precursors to mature collagen and thus reinforce connective tissue. It has been well documented that direct exposure of fibroblasts to growth factors (either endogenous or exogenous) causes new cell growth and collagen deposition. Inflammation creates secondary growth factor elevation. The inflammatory stimulus of Prolotherapy raises the level of growth factors to resume or initiate a new connective tissue repair sequence which had prematurely aborted or never started. Biopsy studies have shown reorganisation of the ligamentous and tendinosseous junctions with patients reporting a reduction in pain and improvement in general range of motion.
Dextrose Prolotherapy and PRP Prolotherapy are designed to stimulate healing, however rely on the body having enough local repair cells available where the injury is. If a joint area has been chronically injured and inflamed over a long period of time a phenomenon called "cellular depletion" occurs. This means there are not very many local repair cells available, they have been used up over time. If cellular depletion has occurred, local repair stem cells will not be available or the available ones will be used up within a few treatments of dextrose and/or PRP Prolotherapy. This is when Biocellular Prolotherapy may be considered, taking good repair cells from the bone marrow (BMA) known to contain adult stem cells, and using this as the “formula” to inject into the injury site.
*DISCLAIMER: Like all medical procedures, they have a success and failure rate. Patient reviews on this site should not be interpreted as a statement on the effectiveness of our treatments for anyone else.