Frequently Asked Questions
About the Procedures – A Regenerative Perspective
Understanding Platelet Rich Plasma
In the Simplest Terms, How Does Stem Cell Therapy Work?
Where Do the Stem Cells Come From?
What is BMAC (Bone Marrow Aspirate Concentrate) and Why?
How Many Treatments Will I Want to Do and How Often Will I Receive Them?
How Soon Might I Notice Improvement?
How Will I Feel Immediately After the Treatment?
PRP – Can you get a Better Result through Higher Platelet Concentration?
What Causes Osteoarthritis (OA)?
About the Procedures
About Platelet Rich Plasma
Platelet rich plasma is a complex composition of cellular components that, when prepared properly, can be used to heal and repair a host of injuries and conditions. Platelet rich plasma is a biologic, and the cornerstone of the consortium of regenerative therapies used in modern medicine. It is chosen over surgery for many conditions, ranging from degenerative joint disease, to tendon and ligament tears.
Platelets are one of several components found in your blood. When your body is injured, platelets rush to the area and stop the bleeding by making your blood clot. The platelets then do another essential job: they activate healing.
Platelets contain growth factors and healing proteins. When platelets release these substances at the site of damaged or diseased tissues, they accelerate healing by:
- Triggering the growth of new tissues
- Preventing the degeneration of healthy tissues
- Reducing inflammation
- Attracting mesenchymal stem cells to regenerate new tissue
PRP contains a higher concentration of platelets than what’s normally found in your blood. When PRP is injected into the site of damaged tissue, the concentrated growth factors go to work, stimulating tissue regeneration and repair.
PRP is made from a sample of your own blood, so it’s completely safe. In most medical offices, your blood is processed in a one-size-fits-all centrifuge that simply separates the platelets from the other blood components. But, the PRP we produce meets a higher standard. For example, treating arthritis requires a very high concentration of platelets, while tendons and ligaments respond better to less concentrated PRP.
PRP is widely used to treat sports injuries, painful musculoskeletal conditions, many professional and recreational athletes credit PRP with enabling them to get back into sport, and patients suffering from chronic pain find they can fully participate in life again.
A few of the conditions we frequently treat with PRP include:
- Osteoarthritis
- Rotator cuff injuries
- Tennis and golfers elbow
- Achilles tendonitis
- Hip tendinopathy
- Joint pain
- Low back and neck pain
- Soft tissue strains/sprains and tears
In the Simplest Terms, How Does Stem Cell Therapy Work?
Every joint in the body and most tissues contain stem cells that are responsible for maintaining health in that location. Degeneration of tissues or joints occur when the stem cell population becomes depleted and that structure losses its ability to regenerate. Stem cell therapy is an attempt to repopulate tissues or joints with stem cell levels reminiscent to when we were 25-35 yoa, thereby restoring the body’s ability to generate a therapeutic process heal itself.
Stem cells are naturally occurring cells in the body that have the potential to turn into other types of cells and body tissues. They also serve an important signaling functioning, recruiting other stem cells to the target area and triggering nearby cells to begin the repair process. In fact, most scientists think that this messenger activity is the main way that stem cells work.
Contrary to what most people think, including most physicians, stem cells do NOTwork their magic by differentiating into new tissue. Instead, they largely act as high-powered messengers that signal other cells–including other dormant stem cells–in and around the damaged tissue to turn on and begin the healing process.
What are the Risks of the Procedures?
There are very few risks involved. You are certain to be sore for a few days after the procedure, but that is a treatment response, not a risk. Infection is the most unlikely serious risk as in any procedure which involves an injection. Regenerative injection therapy and adult stem cell therapy are conservative approaches to treating pain unlike surgery that might help, but it might make it worse. You can always have surgery, but you can’t “un-have” it. The biggest risk of these therapies is that it won’t help your condition, however, performed properly, they will not make your condition worse.
While the use of stem cells is gaining in popularity, it’s important to note that not all stem cell treatments are the same. How the stem cells are obtained and how they’re processed can have a major impact on effectiveness. In addition, even the best stem cell products will be minimally effective if not administered properly. At the Ashmore Osteopathic Group, we use the latest technology to harvest your stem cells to ensure the highest quality product. We also perform all of our injections under direct ultrasound guidance so you can be assured of the safest, most accurate, and most effective treatment.
How is the Procedure Performed?
The Marrow Cellution™ bone marrow aspiration device uses its patented technology to harvest high quality stem & progenitor cells from various levels within the marrow space, while limiting peripheral blood contamination.
https://player.vimeo.com/video/157184256?wmode=opaque
What are Expected Post-Procedure Guidelines?
EXPECT POST-INJECTION SORENESS for 2-5 days following treatment. Although some patients report no increase in pain, you may experience some increase in pain, or “flare”, especially during the first 36 hours after treatment. Our therapies stimulate healing by causing local inflammation, so soreness is a normal response, please do not panic.
DO NOT USE ANTI-INFLAMMATORY MEDICINES for at least 10 days after the treatment. Ice treatment may be used as an analgesic rather than as an anti-inflammatory. Medicines such as aspirin, ibuprofen or Naproxen (either oral or topical) and/or ice stop the inflammatory process that we are intentionally triggering and thus can negate the benefits of treatment. You may use heat for 5-7 minutes at a time along with gentle stretching/mobilisation to relieve discomfort, or alternating hot and cold (3 minutes hot, one-minute cold). Using paracetamol, Tramadol, narcotic pain medicines, or muscle relaxants may also relieve pain without interfering with the effect of the treatment. All-natural supplements including natural anti-inflammatory supplements are OK to take.
IT IS CRITICAL TO REST TO ALLOW YOUR TISSUE TO HEAL. For the first week limit activity to 50% of normal, and the second week, 75% of normal. Avoid repetitive motion, heavy exercise or impact sports for the first 2 – 3 weeks after PRP treatment or 3 -5 weeks for BMAC procedure. Walking, stationary bicycle, and gentle stretches such as yoga are encouraged as tolerated. A common setback is that people will feel better soon after the treatment and then overdo it by deciding to catch up on all the manual activities that need attending to.
Following this would expect a return to normal exercise regime within 5-7 weeks following the procedure. Some activity modification/review of exercise regime may be appropriate.
PLEASE, be VERY CAUTIOUS not to injure yourself in the healing phase.
BONE MARROW ASPIRATION – Keep the marrow extraction site covered and dry for 5-7 days. Following Bone Marrow Aspirate procedure, the incision is covered with a steri strip and tegaderm cover. NO PUBLIC POOL, SWIMMING OR HOT BATHS FOR AT LEAST 5 DAYS.
BE PATIENT WITH THE HEALING PROCESS AND DO NOT HAVE UNREALISTIC EXPECTATIONS. Although some patients notice a reduction in pain within a few days after treatment, more often than not, the regeneration of tissue (up to 3-5 weeks following PRP procedure, and up to 7 – 9 weeks following BMAC procedures) continues for months afterwards. Repeating the treatment after 3-6 months to 1 year may be necessary to optimise benefits, especially for old chronic injuries or advanced, “bone-on-bone” arthritis.
Have realistic expectations and be patient. While we do report that our overall results are excellent, we do not help everyone. If your procedure does not meet your expectations, it is not because we ‘did it wrong’, it’s simply because it doesn’t work for everyone. Even in the best-case scenario, healing and improvement in pain can take up to 3-5 weeks to notice. So, if you are a few weeks out and are not miraculously better, don’t panic. Please be patient, this is not a quick- fix. The progress may be cyclic, but generally always moving forward with a reducing pain scale.
Where Do the Stem Cells Come From?
Upon establishing that you are indeed a candidate for treatment, we will harvest stem cells from your bone marrow, which are then concentrated. (BMAC-Bone Marrow Aspirate Concentrate). The donor and recipient are the same person. Patients who undergo treatment using BMAC do so after careful consideration/consultation by a medical practitioner to determine if the procedure is their best option based on general health/condition of joint regions to be treated and the costs/benefit ratio involved. Based on close follow-up with our previous patients, this appears to provide the most consistent and powerful results.
It’s important to note that currently there is no such thing as a pure stem cell treatment. Derived from bone marrow, the solution that gets injected contains many types of cells, not just stem cells. It also contains healing proteins and growth factors. It’s a total package of stem cells, other cells, and the associated proteins and growth factors that are involved in the healing response.
It is not uncommon to follow up with intra-articular BMAC procedure to problematic joints as needed.
If you have a history of bone or blood cancer, then you may not be a candidate for BMAC procedure.
What is BMAC (Bone Marrow Aspirate Concentrate) and Why?
For the more technically minded:
- The only advantage to not centrifuging is saving time (<15 minutes) and possibly kit costs depending on which needle or kit you use.
- Great aspiration technique (ie. small syringes and small volume draws, may enrich MSCs by 3x, BUT centrifugation can easily achieve another 4x on top of that or 12x above the poor aspiration technique baseline BMA.
- HSCs and platelets are only enriched, while RBCs, clots, and bone fragments are only excluded, by centrifugation.
- Going beyond aspiration and centrifugation, filtration is the only way to further enrich plasma proteins like IRAP (interleukin 1 receptor antagonist protein), A2M ( alpha 2 macro globulin) and fibrinogen. Centrifugation is required to obtain the platelet-poor plasma to enrich plasma proteins in the end product.
- Utilising PRP and Stem Cell procedures have had no infections in hundreds of bone marrow aspirations.
- The BMAC procedure takes approximately 1.5 hour start to finish to have the procedure…including the 20 minute centrifuge time.
- Published literature with human patients where bone marrow was used as a source of stem cells is completely dominated by studies that use bone marrow concentrate and not just bone marrow aspirate.
- Ultimately, with peer reviewed evidence, there may be a place for more orthobiologics that are useful in patient care, but when it comes to bone marrow aspirate, for all of the reasons listed above…..The choice is to concentrate the bone marrow every time.
- Get a higher CFU – colony forming unit count (3x-5x better than a great bone marrow aspiration that doesn’t concentrate)
- We concentrate the plasma proteins
- Able to remove the red blood cells
- Remove any debris
- It takes 1 hour in the office under ultrasound guidance
- There have been no infections and no complications other than occasional soreness more than a day at the donor site from our practice tested single stick technique.
How Many Treatments Will I Want to Do and How Often Will I Receive Them?
Results vary, and unfortunately and sometimes we cannot help everyone even after our best efforts. Based on our overall experience, at the about the 6 month mark after a BMAC treatment, some of our patients are still going strong with 70% or better improvement and do not request a second treatment. Others have had improvement in the 30%-70% range and may request a second treatment, which would include a PRP follow-up. Once we get people where they want to be, most patients may require further treatments every two to three years or on a needs-be basis. Some patients may be “non-responders” and have no improvement at all. Factors may include patient health/habits, adherence to post-treatment guidelines, and severity of the condition.
How Soon Might I Notice Improvement?
These therapies are intended to stimulate the regeneration of connective tissues by altering the tissue signalling. Unlike a steroid injection, there is rarely immediate pain relief. Typically, patients notice improvement after three to seven weeks and continue to notice continual improvement months after the procedure (unlike a steroid injection that typically wears off after a period of weeks or months).
How Will I Feel Immediately After the Treatment?
After the BMAC procedure, you will have localized soreness and discomfort, especially after joint, hand, foot, and shoulder injections. Most patients find over-the-counter medications and rest sufficient to help with the pain. You will be provided with a post-procedure pack containing some short term medication and guidelines to follow.
Are the Results Permanent?
Unfortunately, nothing in this life is permanent. Total joint replacement surgery is not permanent either; even the latest prosthetic devices may eventually require to be replaced. The treatments we offer are intended to alter the tissue signalling in the body to help restore the bodies own innate capacity to generate a therapeutic process, this is what regenerative medicine is basically about. Our overall experience has been that 3-6 months following intra-articular joint BMAC procedure or PRP treatment, patients notice an improvement. But, as mentioned every patients experience and outcome will vary, with majority of patients doing very well and others require secondary follow ups.
PRP – Can you get a Better Result through Higher Platelet Concentration?
While there are many different treatment protocols and a lack of standardisation that exists in the preparation of platelet-rich plasma (PRP), it is important to keep in mind that not all PRP is created equal.
The goal of all PRP is to stimulate the damaged/degenerative region’s natural cells toward repair. Platelet concentration is directly proportional to growth factor concentration. When more platelets are isolated in a PRP preparation, more growth factors are delivered to the application site. These growth factors support several key processes, including stem cell recruitment, angiogenesis, cell proliferation and differentiation – all contributing to cellular regeneration.
It has been demonstrated how stem cells responded when stimulated by platelets from different age groups, as the amount of growth factors in platelets declines with age. For all patient groups (patients in their 30’s, 40’s, and 50’s), a higher concentration of platelet rich plasma stimulates more stem cell growth.
Concentrating in this age group makes a difference. What we are possibly seeing is that there’s a saturation point. This means that when you’re young, you have an abundant amount of growth factors in your platelets, so at some point concentrating them beyond a physiologic limit is a point where the cells are unable to generate a further therapeutic process, referred to as a saturation point.
Regarding growth factors there are two parts to the equation. On the one side you have the amount of growth factors coming from platelets, while on the other there are receptors that these growth factors stimulate on the damaged tissue or local MCS’s. The body frequently adjusts the number of receptors based on a feedback mechanism on cells, up or down, based on what’s available to trigger those receptors. Having less growth factors circulating around them, older stem cells may express more receptors for these platelet growth factors on their surfaces. Having more receptors means they can respond better to less stimulus coming from older and growth factor depleted platelets. Flooding these older cells with lots of platelet growth factors may therefore give an even better proliferation response, as there are more receptors for the GFs to stimulate.
So, concentrating PRP to high levels in older patients is likely well worth the effort. So if you’re middle aged, you may want to take advantage of this additional concentration to maximally stimulate the regenerative process to its full potential.
What Causes Osteoarthritis (OA)?
Osteoarthritis develops when the cartilage, the smooth covering that protects the bones in the joint, breaks down. The surface of the bones becomes damaged, causing pain, swelling, stiffness, and disability. 3 classes of proteins generally referred to as proteases, cause the breakdown of cartilage and lead to the inflammation and pain associated with an arthritic state. The inflammatory response caused by cartilage breakdown accelerates the progression OA and overpowers the body’s natural defenses; the biological mediators intended to protect your joint.
What Are Proteases?
Proteases are enzymes that break down proteins. The proteases that cause cartilage breakdown, joint pain, and Osteoarthritis include 3 proteases classes (Cytokines, MMP’s). The proteases function by breaking down the cartilage cells; causing inflammation, swelling, and pain.
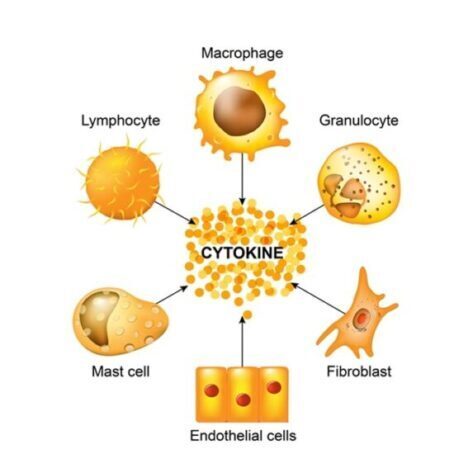
What are Cytokines?
Cytokines are cell signalling molecules that aid cell to cell communication in immune responses and stimulate the movement of cells towards sites of inflammation, infection and trauma. Cytokines exist in protein and glycoprotein forms, include the agents interleukin and the interferon which are involved in regulating the immune system’s response to inflammation and infection.
What are MMP’s?
While cartilage is made up of proteoglycans and type II collagen, tendon and bone are composed primarily of type I collagen.
In OA inflammatory cytokines such as interleukin-1 beta (IL-1 beta) and tumor necrosis factor-alpha (TNF-alpha) stimulate the production of matrix metalloproteinases (MMPs), enzymes that can degrade all components of the extracellular matrix and joint cartilage.
What are Protease Inhibitors?
Protease inhibitors are protein molecules that serve as biochemical mediators to inhibit proteases. Protease inhibitors stop the damaging affects of proteases by binding to and capturing the proteases in the joint and neutralizes their degenerative effect. Protease inhibitors, specifically Alpha-2-Macroglobulin (A2M), inhibit all known causes of cartilage breakdown.
What is Alpha-2-Macroglobulin (A2M)?
A2M is a Broad Spectrum Multi-Purpose Protease Inhibitor with a “bait and trap” mechanism found naturally in the blood. This “bait and trap” mechanism captures and inactivates the proteases damaging the cartilage in your joint. Once these bad proteases are trapped by the A2M, their ability to damage the cartilage is neutralized and the body eliminates them through natural mechanisms. A2M’s protective characteristics designate this vital protein as the human body’s own defense against Osteoarthritis (OA).
Where Does Alpa-2-Macroglobulin (A2M) Come From?
A2M is produced in the liver and found in high concentrations in the blood. Similar to your body increasing white blood cells in response to infection, A2M is unregulated in response to a cartilage injury. The high quantities of A2M found in blood are too large to transport into the joint to provide joint protection from OA. Therefore, supplemental injection of concentrated A2M has the therapeutic potential to stop cartilage breakdown, decrease inflammatory factors, and inhibiting protease activity.
About the Practice and Practitioners
What Is AHPRA?
AHPRA is the Australian Health Practitioner Regulation Agency. AHPRA is the agency that supports the National Boards to implement the National Scheme.
What is the National Scheme?
The National Scheme has a number of objectives, some which include and pertain directly to our scope of practice, including:
- Help keep the public safe ensuring that only health care practitioners who are suitably trained and qualified to practise in a competent and ethical manner are registered. Facilitate provision of high quality education and training for practitioners.
- And, so duly noted that David Krizanic BClinSc/BOSc, Osteopath is Board Certified by AHPRA in performing within the scope of practice as outlined on the Ashmore Osteopathic Group website regarding treatments currently provided.
At present David is currently in the process of obtaining RMSK Certification. The RMSK credentialing program is now accredited by The American National Standards Institute. To earn the RMSK certification, the educational and professional prerequisites must be met and pass the Musculoskeletal (MSK) sonography examination. The MSK examination requires applicants to be licensed, practicing practitioners or advanced care professionals who have clinical musculoskeletal ultrasound experience.
David is an osteopath who has completed a double degree, Bachelor Clinical Science / Bachelor Osteopathic Science at RMIT in 1996 and clinically, began practice treating all manner of musculoskeletal issues using predominantly conventional Osteopathic Manipulative Techniques (OMT).
It was in 2003-2005 as a treating practitioner on the Tour de France where he met a German Orthopaedist who largely used interventional orthobiologic therapies such as Actovegin / Traumeel to treat all manner of sports injuries very effectively (and does so even today). It was here that the concept of incorporating the use of a cellular and a mechanical approach to treating patients with musculoskeletal issues began.
Following on from this he has transitioned his scope of practice which now incorporates the use of these regenerative/orthobiologic therapies for the treatment of many musculoskeletal pain conditions.
To facilitate this, has since undertaken extensive further postgraduate education which has included training in cellular prolotherapy, at the American Academy of Musculoskeletal Medicine. In 2017 completed a fellowship program in Integrative Medicine and Stem Cell Therapies at the American Academy of Anti-Ageing Medicine (A4M). Completed training in phlebotomy, joint puncture and soft tissue injection techniques and protocol, Diagnostic and Interventional Guided Musculoskeletal Ultrasound, MRI assessment with Radiologically Guided Intervention and Emergency Medicine. He actively maintains accreditation with the MSKUS: Musculoskeletal Ultrasound Faculty.
How Do You Know we are in the Right Place?
Imaging is used for 100% of the diagnosis and procedure protocols that are performed; ultrasound for the guided interventions for soft tissues (rotator cuff, achilles tendon, plantar fascia, etc). A needle is never advanced without seeing the exact position of placement and requires a very detailed understanding of anatomy/sonoanatomy to be able to work this way.
All procedures are always performed under the direct supervised protocol of a medical practitioner.
What Guarantee Do I Have That I Will be Satisfied with the Results?
None. We are happy to report that our overall patient satisfaction rate is very high. We grow almost entirely by word-of-mouth referrals from satisfied patients. We help more people than we don’t help, but we don’t help everyone. We have found that the severity of the condition is much less of a predictor of the clinical outcome than is the overall health of the person being treated.
Will I See Improvements in My X-Ray or MRI?
We apologise in advance to the engineers/scientists, we know you may not totally agree this answer. While the goal of stem cell therapy is to reduce your pain and increase your activities of daily living and quality of life, it most likely will not lead to improvements in your X-ray or MRI… and we’re OK with that. To us, success is being able to normally walk down a flight of stairs, keep up with the grandkids, or go surfing. We do not base our treatment outcome on the before and after pictures.
How can stem cell therapy reduce your pain without improving your pictures? In the evaluation of pain, we consider “the subjective” and “the objective”. The subjective is the pain the person reports and the objective are “the pictures”; the diagnostic imaging such as X-ray and MRI. You would think that the two would be directly correlated; the worse the pictures, the worse the pain. But it turns out, it has been proven they are not directly correlated. What this means is how bad the pictures look, does not predict how much pain the person reports. There have been conducted large, scientific studies looking at people with no back pain, and they frequently have abnormal spine MRI’s. We see it all the time in the clinic when we X-ray knees; frequently, the one that looks like “the bad one” doesn’t hurt much, and the one that looks like “the good one” is excruciating. Just because it looks bad, doesn’t mean it’s painful and just because it looks normal, doesn’t mean there’s no pain. How is this? We can think of our bodies in terms of macro-environments and micro-environments. Macro-environment is anatomy that shows up in X-ray or MRI (bones, joints, ligaments, tendons). Micro-environment is the microscopic anatomy that cannot be seen on X-ray or MRI, such as tiny nerves, tiny blood vessels, and collagen fibers. Macro-environments are not the pain generators. Micro-environments are the pain generators. When we inject stem cells into an area, we are treating the micro-environment by altering the tissue signalling which then permits a better orchestrated therapeutic process to reorganise more robust collagen and healthy blood vessels, but most often, we are not altering the gross anatomy.