Introduction
A joint is the union of two bones, regardless of the location in the body. A joint allows controlled movement of bones relative to each other, thus allowing the skeleton to move and endure incredible pressure during movement.
In a healthy joint, the ends of the bones are coated with a thin layer of articular cartilage, reducing friction. These bones are also surrounded by a joint capsule with a tough outer layer (to connect the bones and protect the joint) and a permeable inner layer or synovial membrane. The membrane secretes synovial fluid, a slippery, viscous liquid, which provides essential lubrication, and allows the passage of nutrients and other elements from the bloodstream.
Synovial fluid is nutrient-rich containing proteins, enzymes, water, leukocytes and a key ingredient – sodium hyaluronate, which is responsible for the fluid’s elastoviscous qualities.
Sodium hyaluronate (formerly known as hyaluronic acid) is a glycosaminoglycan (GAG), which arranges itself in complicated coils, adapting to the pressure changes in the joint capsule as we move. It assures the unhindered passage of metabolites to and from tissues throughout the joint, and also serves as a stabilizer and shock absorber for the structures that are undergoing continual, changing mechanical stresses.
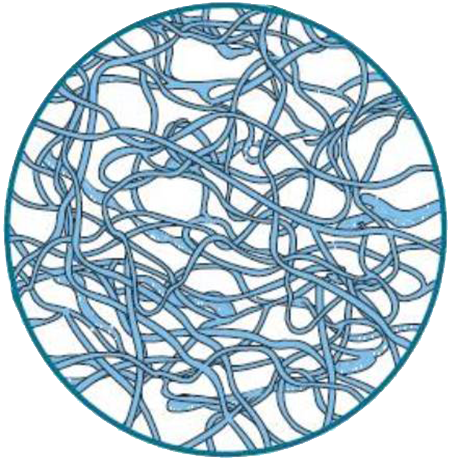
Molecular structure of hyaluronic acid
Articular cartilage, the other main shock-absorbing component of a joint, is an efficient, but flawed structure. Its structural framework is a web of collagen fibres with cells called chondrocytes scattered along the matrix. Chondrocytes produce giant proteoglycan molecules that bind the GAGs. The GAGs, in turn, extract and loosely hold large amounts of water molecules. When cartilage is damaged, there is a decrease in the number of GAGs; therefore, the cartilage holds less water.
Cartilage conforms to the bone surfaces for a tight fit between weight-bearing bones, it spreads pressure evenly over a broad area and manages the water in its matrix, squeezing it out when the joint is under pressure and drawing it back in when the joint is not under pressure.
This in-and-out movement of the fluid transports nutrients throughout the cartilage. However, there is a downside to cartilage as it has no blood or nerve supply of its own, so cartilage has little or no ability to heal or repair itself. Although cartilage performs admirably under normal conditions.
Inflammatory Knee Arthritis
So, what is the underlying reason for joint damage? The answer is quite simple – inflammation.
Inflammation is normally a protective mechanism initiated by the body in response to injury in an attempt to repair the injured tissue. Inflammation causes blood vessels to dilate, and allows fluid and cells to leak out. However, the inflammation response in a joint is a process designed to break down and remove injured or foreign material.
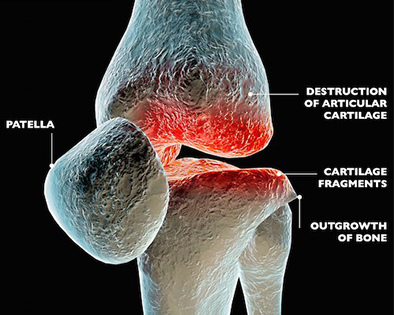
This process changes the chemical makeup of the fluid in the joint, introducing excess fluids, and a high concentration of destructive enzymes and prostaglandins into a closed area (the joint capsule). This destroys the lubricating GAGs and the synovial fluid begins to lose viscosity. The articular cartilage eventually suffers from a compromised nutrient supply, and cannot keep up with repairs and develops damaged areas, opening the bone ends to direct trauma.
The bone responds with a defence that only causes further destruction; it lays down new bone to strengthen the surface (sclerosis) and extends its margins in the form of bone spurs. If left unchecked, this 'runaway inflammation', known as arthritis, will totally destroy the joint.
The term Osteoarthritis is used to describe degeneration of joint cartilage and the underlying bone, most common from middle age onward. It causes pain and stiffness, especially in the hip, knee, and thumb joints.
Treatment Strategies
Many options exist for treating joint disease. The major treatment goals are to reduce inflammation, to improve health of joint fluid and articular cartilage. Treatments to accomplish these goals generally fall into two categories: physical therapies and medical therapies.
Physical therapies include rest, bandaging, application of heat, application of cold and mild, controlled exercise to maintain range of motion.
Medical treatment options for patients with joint disease attempt to replace some of the natural constituents of joint fluid or cartilage, with the hope that the body could use those building blocks to restore normal joint function.
Corticosteroids and hyaluronic acid are the most frequently used intra-articular therapies in osteoarthritis. Other intra-articular substances such as Dextrose / PRP / Cellular Prolotherapy, saline injections, analgesic agents, non-steroidal anti-inflammatory drugs, glucosamine, sodium pentosan polysulfate have been investigated as potentially therapeutic in the treatment of arthritic joints.
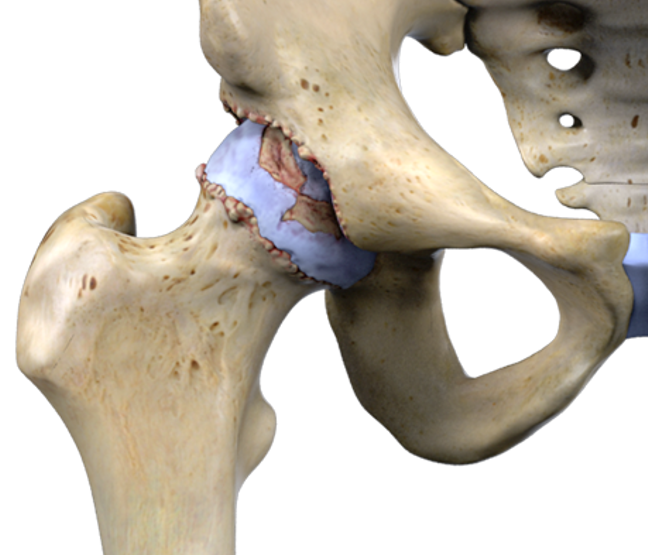
Hip Osteoarthritis
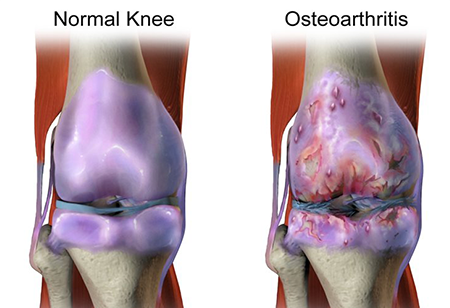
Knee Osteoarthritis
As a practical approach for a knee with effusion, steroid injections should be considered while the presence of symptomatic “dry” knees may favor another approach. The virtual absence of serious side effects, coupled with the perceived benefits, make these other approaches attractive.
An approach that has been considered in conjunction with other approaches is Pentosan Polysulphate (PPS), which was first reported as a chondroprotective drug in 1988. The mechanism of PPS action in osteoarthritis is multifactorial, with both stimulation of cartilage matrix synthesis and prevention of cartilage breakdown and maintained the proteoglycan content in the articular cartilage.
Pentosan polysulfate (PPS) is a semi-synthetic drug manufactured from beech-wood, PENTOSAN INJECTION is a concentrated anti-inflammatory and stimulant of cartilage synthesis, repair and protection. PPS produces an increased amount and quality of hyaluronic acid which results in an increased production of the normally viscous joint fluid.
However, PPS is not a TGA approved drug in Australia. This may change in the near future with clinical trials currently being conducted.
Corticosteroids, anti-inflammatory agents and NSAIDs all relieve the symptoms of osteoarthritis but DO NOT ALTER THE DISEASE PROCESS. Both hydrocortisone and NSAIDs have a marked inhibitory effect on cartilage, which limits the early healing response of cartilage to injury.
References
- Kumagai et al.: Sodium pentosan polysulfate resulted in cartilage improvement in knee osteoarthritis - An open clinical trial-. BMC Clinical Pharmacology 2010 10:7.