Firstly, a lot of literature has been written about Platelet Rich Plasma Therapy, and surprisingly many medical professionals still are not even familiar with it. So, as an introduction we will attempt to explain it in simple terms and what type of conditions it may be able to help, which will then be followed by a more scientific explanation.
Platelet Rich Plasma (PRP)
Platelet-rich plasma, or PRP, is a substance derived from blood that contains a very high amount of platelets, which have a lot of growth hormones and various other healing factors. We can take a little blood from a patient (about the same amount needed for a routine test), put it in a centrifuge, and then inject the PRP directly into an injured area, enabling it to recover at a very accelerated rate.
How We Create PRP
With PRP, we draw a sample of blood in our office, just like having a standard blood test. Then, while you wait, we process your blood to extract and concentrate the platelets. We then inject the platelet concentrate directly in the damaged area(s). The platelets release their growth factors and the healing begins.
How PRP Therapy
Can Help You
PRP treatment works best for chronic ligament and tendon sprains/strains that have failed other conservative treatment, including:
- Rotator cuff tears,including partial-thickness and full-thickness tears
Rotator cuff tears can range from very small tears all the way to massive complete tears. While surgery traditionally has been the main treatment for cuff tears, treatments such as PRP and stem cells can be excellent alternatives. However, if you have a massive complete tear then Regenerative Medicine treatments usually don’t help.
- Shoulder pain and instability
- Tennis and golfers elbow
Tennis Elbow and Golfer’s Elbow technically are known as lateral epicondylitis and medial epicondylitis, respectively. They are a type of chronic tendinitis. Causes of Epicondylitis most commonly include any repetitive stress over time. However, an acute injury can also damage the tendon. Symptoms of Epicondylitis typically include pain and tenderness over the point of the elbow, pain or weakness when trying to grasp or pick up objects, or pain when performing certain tasks.
- Hamstring and hip strains
- Knee sprains and instability
Understanding Knee Instability
The structures on the medial, antero-medial and postero-medial side of the knee are medial compartment structures and stabilisers and structures on the respective lateral side are lateral compartment stabilisers.
The contribution that both muscles and ligaments make to stability is dependent on joint position of the knee and the surrounding joints, the magnitude and direction of the force and the availability of reinforcing structures to resist forces if the primary restraints become incompetent.
The ACL consists of two functional bundles, the antero-medial bundle and a stronger thicker postero-lateral part. In extension the postero-lateral bundle is taut. In flexion the antero-medial band becomes tight and the bulk of the ligament slackens. In flexion it is the antero-medial band that provides the primary strength against anterior displacement of the tibia.
The PCL consists of two inseparable parts. An anterior part forms the bulk of the ligament and a small posterior part runs obliquely to the back of the tibia. In extension, the bulk of the ligament is relaxed and only the posterior band is tight. In flexion a major part of the ligament becomes tight and a small posterior band is loose.
The ACL is a check against both hyperextension and internal and external rotation. The PCL is a check against posterior instability in the flexed knee but not against hyperextension, provided that the anterior cruciate ligament is intact.
As can be seen from the above discussion, the knee joint function is dependent upon static and dynamic factors. In general terms, the static factors can not be influenced in the normal knee, eg the bony geometry or ligament size and position. The dynamic structures however can be influenced and are of vital importance in normal knee joint function. The muscles can be strengthened with appropriate training regimes. Certain static deficiencies can be overcome by appropriate strengthening and training of the dynamic component of the knee. For example, in an anterior cruciate deficient knee, strengthening of the quadriceps and hamstring mechanism along with appropriate co-ordination training can control instability to allow the person to undertake various low risk sports and certainly will control antero-posterior instability. However, even with dynamic muscular training with an absent ACL, rotation stability cannot be offset by muscular training and so the knee will still be prone to giving way with twisting on the weight bearing ACL deficient knee.
The majority of rehabilitation regimes following injury and surgery to the knee emphasise the importance of training and strengthening the dynamic stabilisers to the knee and this is particularly important in patello-femoral pain syndromes where the muscular control of the patella is vital.
- Patellofemoral Syndrome and patellar tendinosis
Chondromalacia patella, also known as Patellofemoral Syndrome is a specific type of knee arthritis that affects the cartilage on the back of the kneecap (the patella). The name "chondromalacia" comes from chondro, referring to cartilage, and malacia, meaning softening or irritation. However, it's important to note that you can have Patellofemoral Pain Syndrome (PPS) without having the cartilage damage seen in Chondromalacia Patella.
Symptoms of
Chondromalacia & PPS
Patients typically complain of pain around or behind the kneecap. Symptoms are worsened by physical activity, especially running and jumping. Prolonged sitting causes pain when attempting to stand back up. Also, going downstairs or inclines can cause pain, more so than going up. Some patients report grinding, catching or locking behind the kneecap. Swelling can also occur.
Causes of
Chondromalacia & PPS
The kneecap sits in a shallow groove (the trochlea) at the lower end of your thigh bone, the femur. Both the back of the kneecap and the surface of the femoral trochlea groove are covered with a thin layer of cartilage that allows the kneecap to glide smoothly and freely within the groove when you bend your knee. But in some people, the kneecap doesn't track evenly in the groove, and it starts to get pulled off towards one side (usually towards the outer side). This is referred to as lateral tracking. This starts to cause uneven wear and irritation of the cartilage surfaces.
The causes of lateral tracking are many. Flat feet can allow the knees to rotate inward, resulting in a greater lateral pull on the patella. Weakness of the gluteus medius muscle (which is a hip/thigh rotator) can also allow the knee to rotate inward. In women in particular, wider hips result in a greater inward angulation of the lower leg (known as the Q-angle), and this can increase the chances of lateral tracking. Most physical therapists and physicians think that weakness of the inner muscle of the quadriceps, the vastus medialis oblique, or VMO, is the contributing cause of chondromalacia/PPS. But it is NOT!
The stability of the knee joint is dependent upon static and dynamic factors. The static stabiliser includes passive structures such as the knee joint capsule and the various ligaments and other associated structures such as the menisci, the coronary ligaments, the menisco-patella and patello-femoral ligaments. The ligaments which all act as static stabilisers include the medial collateral ligament, the lateral collateral ligament, the ACL, PCL, the oblique popliteal and arcuate ligaments. The ilio-tibial band is also considered a static stabiliser in spite of its muscular connections. The bony geometry also contributes to the static stability of the knee. The contribution is variable but can be made worse by certain anatomic variants such as a flat lateral femoral trochlea which will predispose to lateral instability of the patella.
The dynamic stabilisers of the knee are all the muscles and their aponeuroses including:
– quadriceps femoris and extensor retinaculum
– pes anserinus
– popliteus
– biceps femoris
– semi-membranosis.
Treating
Chondromalacia & PPS
Ideally, treating CM/PPS should target the underlying cause(s). Biomechanical problems, such as flat feet, should be addressed.
Dysfunction of the gluteus medius muscle needs to be addressed when present. The problem is that the vast majority of physical therapists don't know how to train the gluteus medius properly to perform its stabilizing function. They instruct patients in high load strengthening exercises. But this isn't the main problem. The real problem is that the gluteus medius doesn't fire in the proper timing sequence, it's not a strength-weakness issue. Delayed contraction of the muscle allows the knee to rotate inward. So therapy needs to work on retraining muscle firing patterns, not strengthening the muscle.
Patellar stabilizing braces and straps to help control patellar tracking can be useful to keep the symptoms under control, but they do nothing to fix the underlying problems. Special patellar taping techniques, such as McConnell Taping, to help control patellar tracking can also be helpful to control symptoms.
When conservative measures such as physical therapy, orthotics, and bracing/taping don't help, more aggressive treatment may be needed. We've had very good success using PRP and stem cell injections. These treatments are intended to stimulate the body's natural healing and repair mechanisms to heal the damaged cartilage and to tighten the ligaments that stabilize the patella. It's important to keep in mind that biomechanical problems and muscle imbalances still need to be fixed - Regenerative Medicine treatments complement these treatments; they don't replace them. Surgery is always a last resort for treating Chondromalacia.
- Ankle sprains
- Achilles tendinosis & plantar fasciitis
Causes of
Achilles Tendinitis
Causes of Achilles Tendinitis are repetitive overuse or by recurring microscopic tears. Less common causes are from steroid use, and from certain medical conditions such as undiagnosed or poorly controlled Thyroid Disease. Sometimes the tendon completely ruptures, in which case surgery needs to be considered.
Symptoms of
Achilles Tendinitis
Symptoms of Achilles Tendinitis include pain and/or stiffness in the Achilles during or after activity, thickening or swelling of the tendon, nodule formation in the tendon (it looks like a marble stuck in the middle of the tendon), and tenderness when squeezing the tendon.
- Knee, hip, and other joint osteoarthritis
- Sports hernias & athletic pubalgia
- Other chronic tendon and ligament problems
- Nerve entrapment syndromes, such as Carpal Tunnel Syndrome ?
PRP can be very helpful for many cases of osteoarthritis (the “wear & tear” kind). PRP can help stimulate a “smoothing over” of the roughened and arthritic cartilage, reducing the pain and disability of arthritis. This includes:
- Knee arthritis
- Hip joint arthritis
- Shoulder arthritis
- And other joint arhtopathies
- And other joint arthritis
Because it uses your own blood, PRP is very safe. Conditions that can be treated effectively with PRP include: Rotator Cuff damage, Tennis & Golfer’s Elbow, Achilles Tendonitis & Plantar Fasciitis, joint pain, arthritis, neck, and back pain (including disc problems), and most sprains and strains.
The scientific literature is full of reports of soft tissue injuries treated with PRP including tendinopathy, tendinosis, acute and chronic muscle strain, muscle fibrosis, ligament sprains and joint capsular laxity, in addition to various degenerative disorders in your joints. PRP has also been shown to be effective for labral tears of the hip and labrum tears of the shoulder joint, as well as degenerated meniscus and meniscal tears. Most recently research has shown PRP to be an effective treatment for mild-moderate joint osteoarthritis.
Platelet Rich Plasma

“The convincing background of the recent studies, investigating the different potentials of platelet-rich plasma, offers the clinician an appealing alternative for the treatment of cartilage lesions and osteoarthritis. Recent evidences in literature have shown that PRP may be helpful both as an adjuvant for surgical treatment of cartilage defects and as a therapeutic tool by intra-articular injection in patients affected by osteoarthritis.”(1)
A patient will often explore non-surgical methods of joint repair after they have been to a doctor that is recommending surgery. When they return to that doctor with questions about PRP they may hear that PRP is unproven, doesn’t work, no research to support it.
Platelet Rich Plasma Therapy is very promising BUT calls for a standardisation for practitioners who want to use Platelet Rich Plasma Therapy (PRP) in the treatment of chronic joint pain. Research and similar papers indirectly and clearly suggest that therapeutic results will vary depending on the level of experience and training the practitioner has in utilising PRP.
The lack of standardisation is discussed in the medical journal Odontology by researcher Tomoyuki Kawase of Niigata University in Japan, and this is clearly alluded to in the research:
- Platelet-rich plasma has been widely investigated and applied to regenerative medicine.
- PRP use is supported by evidence that PRP contains high concentrations of platelet-related growth factors and normal concentrations of plasma-derived fibrinogen, both of which contribute to the regenerative process.
- Additionally, its superior cost-efficacy versus conventional therapies is attractive to many clinicians.
- However, current disadvantages of PRP include a relatively complicated preparation procedure and practitioners effectiveness in giving PRP treatment.(2)
An article in Orthopedics Today from the Hospital of Special Surgery in New York also warns against the high degree in variability among practitioners who use Platelet Rich Plasma (PRP). The main concerns are again those cited above – lack of standardization in treatment regimes and formula concentrations. Also mentioned are the various brands, concentrations, doses, etc that make it hard to determine the best use of PRP.(3)
Doctors in Italy at the Rizzoli Orthopedic Institute and the University of Bologna expressed concern over the lack of standardization among doctors using Platelet Rich Plasma therapy in their study. The researchers do acknowledge that the role of PRP in bone, tendon, cartilage, and ligament tissue regeneration has been shown in numerous preclinical studies published within the last 10 years to have delivered very promising results but many key questions remain unanswered and controversial results have arisen.
Writing in the medical journal Biomed Research International they also call for studies to define the dosing, timing, and frequency of PRP injections, different techniques for delivery and location of delivery, optimal physiologic conditions for injections, and the concomitant use of additional growth factors, biological scaffolds, and combined use of PRP and Stem Cells to develop optimal treatment protocols that can effectively treat various musculoskeletal conditions.(4)
PRP’s best chance to work to its maximum benefit is when it is offered as part of a comprehensive joint regeneration program. That generally means more than one injection/treatment site as well as utilising direct action techniques to restore function to joints. At Ashmore Osteopathic Group we offer PRP treatment as part of a comprehensive Prolotherapy program, that treats all components of the ligament,tendon,cartilage and degenerative joint complex.
All treatment protocols are monitored under the guidance and professional supervision of a medical practitioner working within the scope of this practice.
What is Platelet Rich Plasma Therapy?
PRP therapy is an injection treatment which re-introduces your own concentrated blood platelets into areas of chronic joint deterioration.
Your blood platelets contain growth and healing factors. When collected then concentrated using a specific collection kit and simple centrifuging, your blood plasma becomes “rich” in healing factors, thus the name platelet 'RICH' plasma. Platelets play a central role in blood clotting and wound/injury healing.
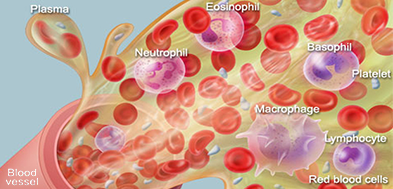
Circulating Blood
The procedure and preparation of therapeutic doses of growth factors consists of an autologous blood collection (blood from the patient), plasma separation (blood is centrifuged), and application of the plasma rich in growth factors (injecting the plasma into a designated region). Initially three to five visits may be necessary per area. In practice, patients may generally be seen every 3-5 weeks.
Chronic complex musculoskeletal injuries that are slow to heal pose challenges to many practitioners. So, the use of orthobiologics is a relatively new science that involves application of naturally found materials from biological sources (blood platelets), and offers exciting new possibilities in the science of regenerative medicine.
Platelet-rich plasma (PRP) is an orthobiologic that has recently gained popularity as an adjuvant treatment for musculoskeletal injuries. . . The relative ease of preparation, applicability in the clinical setting, favorable safety profile and possible beneficial outcome make PRP a promising therapeutic approach for future regenerative treatments.
As PRP gains popularity and more research validates its usefulness and reliability to patients, it is important to remember that PRP is just one proliferate available for regenerative injection therapy. Utilising these numerous regenerative treatments depends on the severity of the pain or injury and extent of degenerative joint changes. This may include Dextrose Prolotherapy, PRP and/or Stem Cell Procedure that all provide a regenerative treatment approach that has proved to be safe and effective.
Platelet Rich Plasma (PRP)
Platelet Rich Plasma (PRP) is an orthobiologic isolated from whole blood that is preferentially enriched for platelets. While platelets are the primary component of PRP, preparations may also contain other cellular components such as a white blood cells (monocytes), lymphocytes and <1% of circulating peripheral blood mesenchymal stem cells (PBMSC). These components all play a biological role in the therapeutic process which are provided at concentrated levels in PRP.
Orthobiologics is a relatively newer science that involves application of naturally found materials from biological sources (blood platelets ), and offers exciting new possibilities to promote and accelerate bone and soft tissue healing.
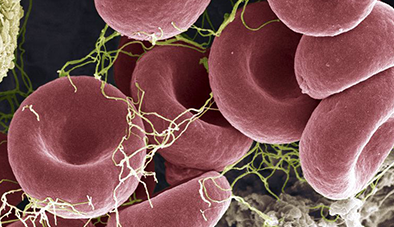
Circulating Platelets
Activated Platelets
Platelets are small, colourless, disk-shaped cell fragments lacking a nucleus that are found in blood and play an imperative role in clot formation and the release of growth factors, it is these growth factors that orchestrate the key biological processes required for the reorganisation of the connective tissue field. Most importantly, the growth factors, including PDGF (The most important specific activity of PDGF is the creation of cartilage), TGF-β, VEGF and SDF-1α are the key to regulating biological activity, including angiogenesis, inflammatory resolution and tissue regeneration.
Growth factors derived from these platelets are responsible for soft tissue, cartilage repair, bone regeneration, development of new blood vessels and stimulation. Research shows that the optimal concentration required is 6-8x the base value of platelets in PRP to optimise the regenerative process and healing.
It is this key point which shows why not all PRP treatments are alike, and very much dependant on the extraction/harvesting process to achieve this critical platelet concentration.
What to Expect..
The benefits may not be noticed anywhere from 3-5 weeks following the first Prolotherapy treatment. Treatment protocol varies from patient to patient, so a patient with advanced degenerative joint changes may expect to be treated with upto 3 PRP injections initially, once every 3 weeks, then in 5 weeks, followed by another in 7 weeks. This subjective to progress and any possible adverse reactions. Hence if you suffer moderate pain, a realistic expectation is it will reduce to mild, mild to none and severe to moderate.The less severe the osteoarthritis, the longer the effect. Following this, patients may still have reduced pain for up to 2 years.
Side Effects..
Common adverse effects can include knee pain or swelling & bruising at either injection site for up to 36-48 hours. Most patients injection site will have varying degrees of discomfort the next day. Severe complications, such as infection are very rare. Pain after the injection is almost always inflammation and/or needle flare..
-
Marmotti A, Rossi R, Castoldi F, Roveda E, Michielon G, Peretti GM. PRP and articular cartilage: a clinical update. BioMed research international. 2015 May 5;2015.
-
Kawase T. Platelet-rich plasma and its derivatives as promising bioactive materials for regenerative medicine: basic principles and concepts underlying recent advances. Odontology. 2015 Jun 4.
-
“Platelet-rich plasma promises pain relief and healing, but remains controversial” Orthopedics Today. Web. April 2013. Accessed April 29 2013.
-
Salamanna F, Veronesi F, Maglio M, Della Bella E, Sartori M, Fini M. New and Emerging Strategies in Platelet-Rich Plasma Application in Musculoskeletal Regenerative Procedures: General Overview on Still Open Questions and Outlook. Biomed Res Int. 2015;2015:846045. Epub 2015 May 5.